What is cancer?
Cancer is a condition in which cells in the body grow abnormally or out of control. Normally, cells grow and divide to create new cells as they are needed to keep the body healthy. Sometimes, this process of growing new cells does not work properly and cancer forms. Since cancer can start any place in the body, there are more than 100 different types of cancer.
How does cancer start?
Normal cells become cancer cells because of damage to a cell’s DNA. DNA is in every cell and directs all its actions. In a normal cell, when DNA gets damaged, the cell either repairs the damage or the cell dies. In cancer cells, the damaged DNA is not fixed, and the cell does not die like it should. Instead, this cell goes on to continue making new cells that the body does not need.
How does cancer grow?
Abnormal cells can grow into a mass, or a tumor. Not all tumors are cancerous. Tumors can be either malignant (cancerous) or benign (non-cancerous). A malignant tumor, or cancer, can spread to other parts of the body and form other tumors. Some cancers, like leukemia, rarely form tumors. Instead, these cancer cells are in the blood and blood forming-organs, and flow through other tissues where they grow. Some cancers grow quickly while others may grow slowly over many years.
What are the signs and symptoms of cancer?
Signs and symptoms are signals that something is not right in the body. Because cancer can start at any place in the body, it can cause almost any sign or symptom to occur. Cancer signs and symptoms will vary based on where the cancer is located in the body, how big it is, how much it affects the organs or tissues, and whether it has spread. Some examples of general signs and symptoms of cancer include unexplained weight loss, fever, extreme tiredness, pain, or skin changes. Having these symptoms does not mean you have cancer, but they are signals that something might be wrong in your body, and should be checked by a health care provider.
It is very important to pay close attention to your body and any signal that something might not be right. This is especially important for cancer signs and symptoms because treatment for cancer works best when the cancer is found early.
American Cancer Society. (2020, February 28). Signs and Symptoms of Cancer. www.cancer.org/cancer/cancer-basics/signs-and-symptoms-of-cancer.html
It is very important to pay close attention to your body and any signal that something might not be right. This is especially important for cancer signs and symptoms because treatment for cancer works best when the cancer is found early.
American Cancer Society. (2020, February 28). Signs and Symptoms of Cancer. www.cancer.org/cancer/cancer-basics/signs-and-symptoms-of-cancer.html
What are the risk factors for cancer?
There are many different risk factors for cancer—some that can be controlled through lifestyle changes, and others that cannot, like a person’s age, family history, or genetics. Behaviors and exposures that may contribute to an increased risk of cancer include:
In addition to behaviors, social and economic factors as well as the physical environments in which a person is born, lives, plays, and works play a critical role in one’s opportunity to achieve optimal health.
Socio-economic and environmental barriers, known as social determinants of health, are factors that deny many people the opportunity to practice healthy behaviors and access quality health-related services. These factors result in health disparities—preventable differences in opportunity and health outcomes between segments of a population. DC Health identifies nine key social determinants of health operating in the District: education, employment, income, housing, transportation, food environment, medical care, outdoor environment, and community safety.
District of Columbia. (2018). Health Equity Report: District of Columbia 2018. dchealth.dc.gov/publication/health-equity-report-district-columbia-2018
- Smoking and other uses of tobacco
- Diet low in fruit and vegetables, or high in processed foods
- Lack of regular physical activity
- Obesity
- Alcohol use
- Sun exposure
- Environmental exposures (lead and asbestos)
- Exposure to infections such as hepatitis, HPV, or HIV
In addition to behaviors, social and economic factors as well as the physical environments in which a person is born, lives, plays, and works play a critical role in one’s opportunity to achieve optimal health.
Socio-economic and environmental barriers, known as social determinants of health, are factors that deny many people the opportunity to practice healthy behaviors and access quality health-related services. These factors result in health disparities—preventable differences in opportunity and health outcomes between segments of a population. DC Health identifies nine key social determinants of health operating in the District: education, employment, income, housing, transportation, food environment, medical care, outdoor environment, and community safety.
District of Columbia. (2018). Health Equity Report: District of Columbia 2018. dchealth.dc.gov/publication/health-equity-report-district-columbia-2018
Should I be tested for cancer?
Listed below are cancer screening recommendations based on The US Preventative Service Task Force Guidelines. It is recommended that you talk to your doctor about your risk factors and discuss your personal screening decisions.
Breast Cancer Screening
Ages 50-74
- Screening Mammogram Every 2 Years
Cervical Cancer Screening
Ages 21-29
- Pap Test alone every 3 years
- Pap Test alone every 3 years
- Pap Test with high-risk human papillomavirus (hrHPV) every 5 years (co-testing)
- High-risk human papillomavirus (hrHPV) only every 5 years
Colorectal Cancer Screening
Ages- 45-75
- Colorectal Cancer Screening test. To learn about different screening test options visit- https://www.cdc.gov/cancer/colorectal/basic_info/screening/tests.htm
Lung Cancer Screening
Ages 50-80
- Annual screening for lung cancer with low-dose computed tomography (LDCT) for adults who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years.
Prostate Cancer Screening
Ages 55-69
- Men should make an individual decision about whether to be screened after a conversation with their clinician about the potential benefits and harms.
- Screening is not recommended, the potential benefits do not outweigh the expected harms.
Skin Cancer
Ages 6 months -24 years
- Counseling about reducing ultraviolet radiation exposure with fair skin types
- There is currently not enough evidence to recommend routine skin cancer screening (total body examination by a doctor) for people who do not have a history of skin cancer and who do not have any suspicious moles or other spots. Report any unusual moles or changes in your skin to your doctor. Also talk to your doctor if you are at increased risk of skin cancer.
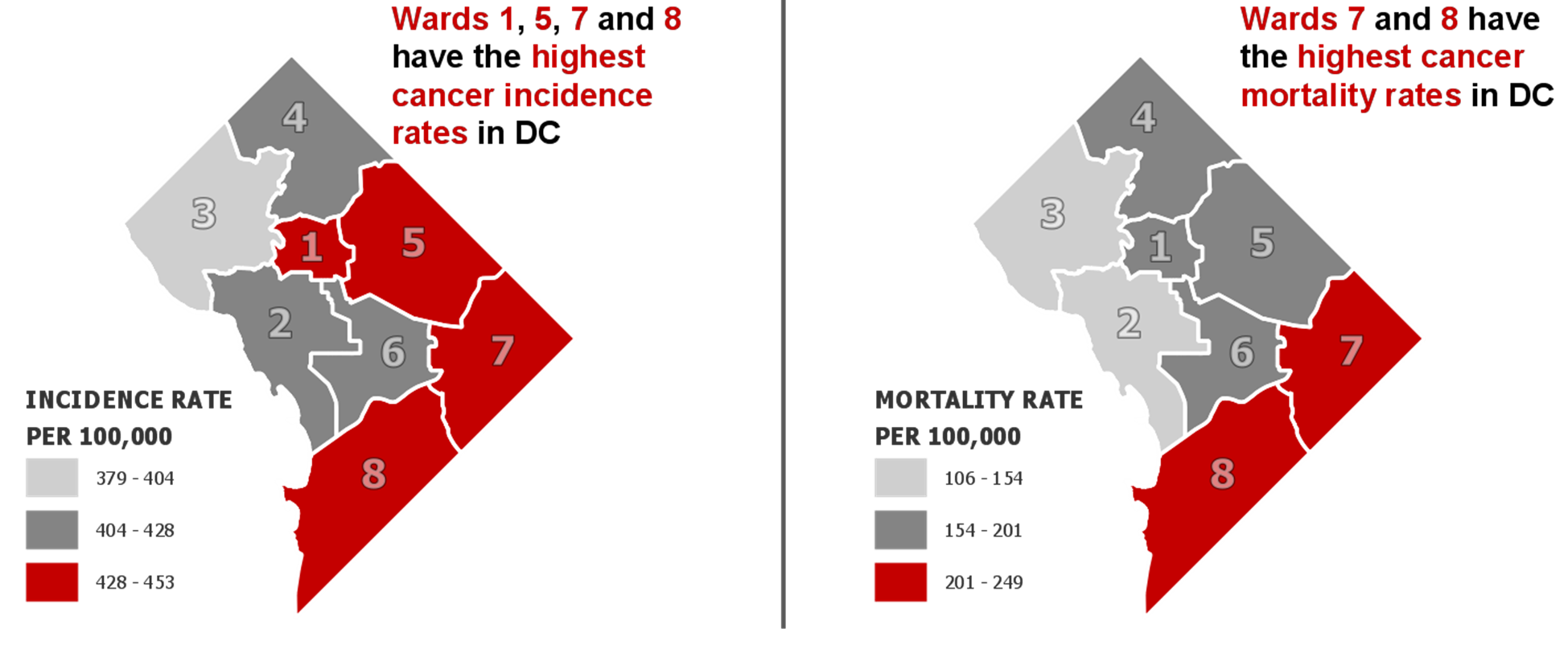
Cancer burden
Cancer is the second leading cause of death in the District of Columbia. The sites of cancer leading to the greatest number of deaths in the District are prostate, lung, breast, and colon/rectum. The highest cancer incidence and mortality rates are seen among residents of Wards 5, 7, and 8 as well as residents who are African American.
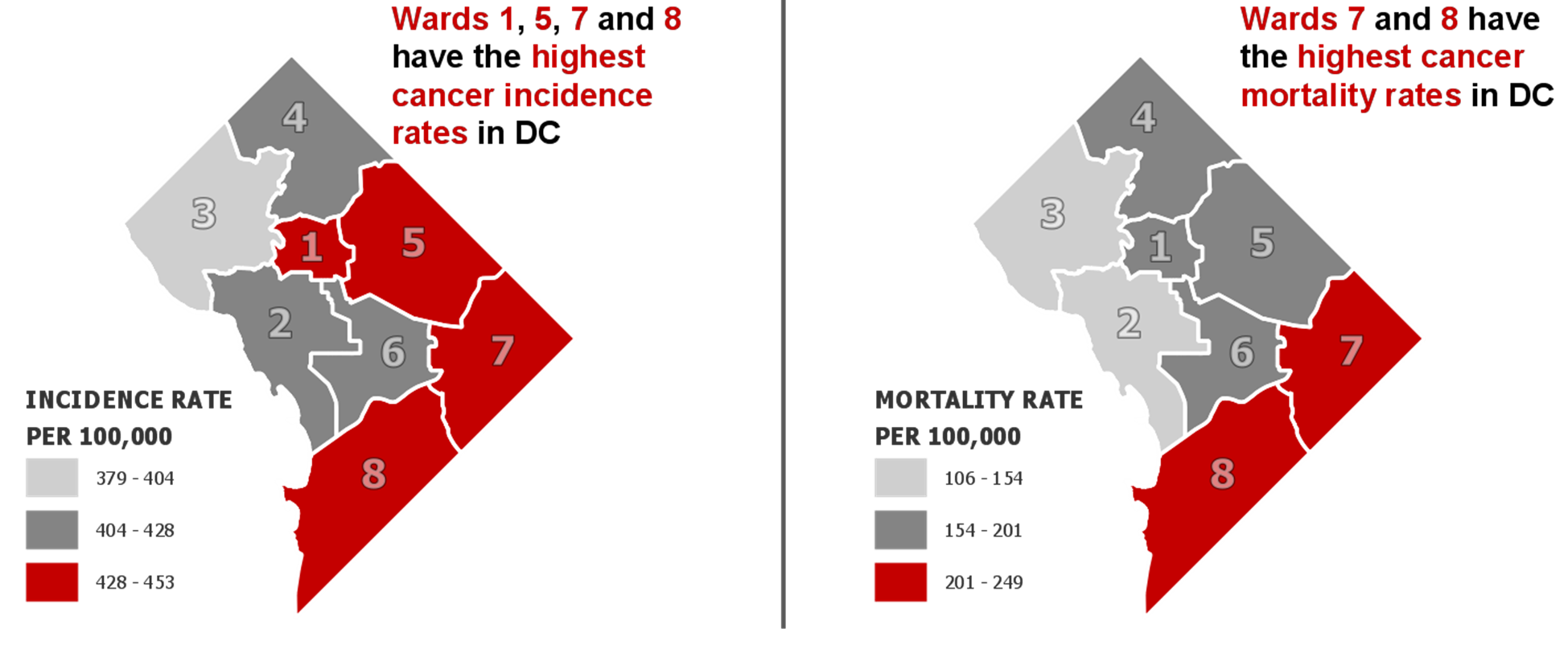
For more information on cancer burden, see the Cancer in DC Fact Sheets here dchealth.dc.gov/service/cancer
For more information on cancer burden, see the Cancer in DC Fact Sheets here dchealth.dc.gov/service/cancer
How can I reduce my cancer risk?
There are several steps one can take to reduce their risk of developing cancer. Cancer risk can be reduced by avoiding tobacco use, eating a diet that avoids processed foods but is rich in fruits and vegetables, maintaining a healthy weight, exercising regularly, getting timely cancer screenings, and avoiding environmental risks such as the sun or chemicals.
Cancer genomics
Genetic mutations have been found to increase a person’s risk of developing certain types of cancers. Inherited genetic mutations are associated with as many as 5% to 10% of all cancers. In DC, African Americans have a higher percentage of family history of any cancer, however genetic testing among African-Americans is less than optimal. Screening for genetic mutations and use of an individual’s family history can help to identify those at higher risk for several cancer types.
Survivorship
DC Health is committed to enhancing survivorship services. Through the Cancer Thriving and Surviving Program services are provided to both survivors and caregivers of individuals diagnosed with cancer. DC Health. (2022). Living Well DC. livingwell.dc.gov/node/1484426
DC Cancer Coalition
The DC Cancer Coalition is a multidisciplinary group of stakeholders interested in reducing the District’s cancer burden by collectively identifying and addressing gaps in cancer services. Guided by the best available evidence, as well as local and national data and the District of Columbia Cancer Control Plan, the Coalition supports programs and policies to reduce the burden of cancer in the District of Columbia.
Mission
To reduce the burden of cancer by improving the infrastructure that supports the equitable delivery of evidenced-based and culturally appropriate education, prevention, screening, treatment and survivorship services.
Get Involved
Contact the Comprehensive Cancer Control Program Coordinator at [email protected] or (202) 442-9212 to learn more or become involved in the Cancer Coalition.
- በዚህ ገጽ ላይ የተተረጎሙ መረጃዎችን በአማርኛ ማግኘት ይችላሉ።
- 請在此處查找本頁信息的中文翻譯。
- Veuillez trouver une traduction française des informations sur cette page ici.
- 여기에서 이 페이지의 정보에 대한 한국어 번역을 찾으십시오.
- Encuentre una traducción en español de la información en esta página aquí.
- Vui lòng tìm bản dịch tiếng Việt của thông tin trên trang này tại đây.